About the Studio
Our Little Venice Studio specialises in Classical Pilates – available as 1-1, 2-1 and small group classes – Physiotherapy and Massage therapy.
Working on a selection of Classical Pilates equipment in private sessions or small group classes of no more than four, clients will discover a friendly and tranquil environment in which to safely and effectively transform their bodies, under the attentive guidance of some of the most qualified Pilates Instructors in London.
For those with injuries and conditions that need a little extra care, you can also expect the same calibre of welcoming and expert care from our onsite Physiotherapists and Massage Therapists as you'll find in any Ten Physiotherapy Clinic.

Pilates at Little Venice combines all the body-sculpting, movement-refining, pain-reducing and posture-enhancing benefits of the Classical Pilates Method with Ten’s trademark focus on the latest insights from exercise science.
Drawing upon their vast experience of working with hundreds of clients, our highly-experienced Pilates Instructors will provide you with a personalised experience tailored to your unique needs, with careful consideration of any biomechanical or other health concerns.

What to expect:
After an initial Pilates Screening your Instructor will create a focused programme tailored to your body. You will then progress to 1-1, 2-1 or small group classes depending on your individual needs and preferences.
Book your Assessment Make an Enquiry
Results and Benefits:
Backed by the latest movement science and with a focus on precision and detail, through tailored, personal Pilates training you can expect immediate and lasting effects including:
- Full body strengthening and sculpting
- Improved flexibility and mobility
- Strengthened joints and injury prevention
- Improved balance, coordination and body awareness
- Decreased back pain and speedier recovery from injury
- Better posture and core strength
-

Mat Pilates
– 1-1/Private
– Small Group Class (Max 4)Mat Pilates
A mix of traditional Mat Pilates and Ten’s advanced movement techniques, this floor-based form of Pilates is the perfect way to understand and develop the basic principles and techniques of Pilates. It’s particularly suitable for anyone with back problems, poor balance or low muscular strength.
-
Classical Pilates
– 1-1/Private
– 2-1
– Small Group Class (Max 4)Classical Pilates
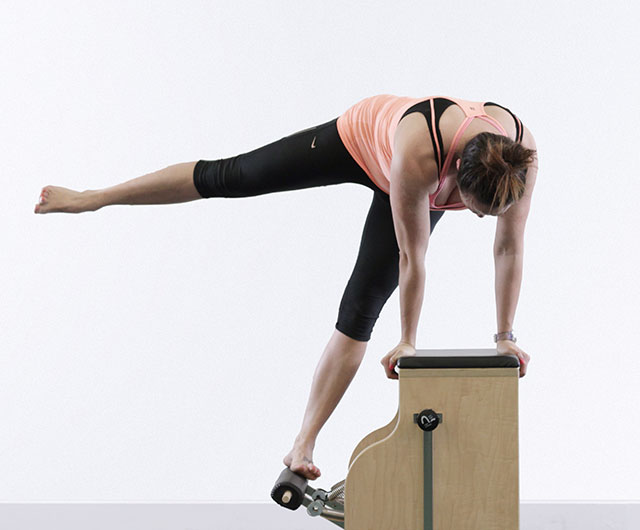
This session uses cutting edge Pilates equipment, including the Reformer, Ladder Barrel, Wunda Chair and Cadillac, to help isolate and treat specific issues and target parts of the body neglected in other forms of exercise.
-

Pre & Post Natal Pilates
– 1-1/Private
– Small Group Class (Max 4)Pre & Post Natal Pilates
These floor and equipment based sessions provide a gentle and effective way to prepare the body for the physical demands of giving birth, and support recovery afterwards.













